Diabetic Gastroparesis: How Does Delayed Gastric Emptying Affect
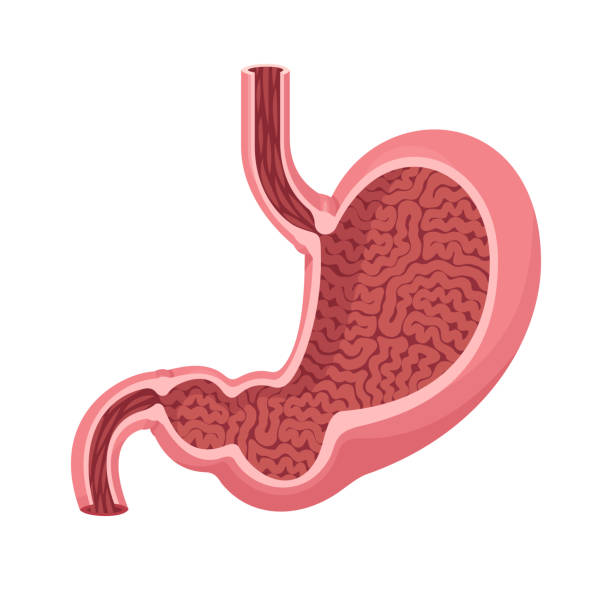
In patients suffering from gastroparesis, the stomach contraction is diminished, elongating the time food spends in the stomach before being expelled into the intestine. Diabetes happens to be one of the causes of gastroparesis in humans.
This article discusses the topic: diabetic gastroparesis, its causes, symptoms, diagnosis, and other vital aspects of the condition.
What is Diabetic Gastroparesis?
Besides diabetes, there are other causes of gastroparesis. However, diabetic gastroparesis simply refers to when the condition is caused by diabetes. According to a report, diabetic gastroparesis is a severe complication of diabetes associated with obstructions of the digestive tract, observed as delayed gastric emptying.
Gastroparesis is not limited to either type of diabetes, as type 1 and type 2 diabetes can be responsible for this disorder. Poor management of diabetes may lead to damaging the vagus nerve.
The vagus nerve controls the peristaltic movement of food in the stomach. When diabetes starts to hamper this nerve, the muscles responsible for the contraction of food in the stomach and other parts of the alimentary canal begin to lose their functions, resulting in this condition.
Why is Gastroparesis Called Delayed Gastric Emptying?
Gastroparesis is referred to as delayed gastric emptying because that’s exactly what happens in the condition. The condition prevents the contraction of muscles of the digestive tract, resulting in delayed stomach emptying of food into the small intestine.
Signs and Symptoms: What is the Effect of Gastroparesis on Digestive Tract and Stomach Muscles?
Most of the signs and symptoms of gastroparesis are related to the digestive system. However, just like any health condition, the signs and symptoms of gastroparesis may vary among different individuals.
Below are a series of symptoms associated with the metabolic condition.
- Nausea
- Heartburns
- Abdominal pain
- Vomiting of undigested food
- Early satiety- feeling full after smaller meals
- Abdominal bloating
- Weight loss
- Acid reflux
- Irregularities with blood glucose levels
- Loss of appetite
- Stomach spasms, etc.
The severity of the damage to the vagus nerve is responsible for the seriousness of these conditions. Also, symptoms are more likely to occur after taking a diet high in fibers or fats, as these foods typically take longer to digest.
The common complications of diabetes often talked about include vision problems, slowed healing, and kidney and heart-related disorders. However, it is essential to note that gastroparesis is a severe complication of diabetes. Hence, the need for diabetic patients to visit the hospital for regular checkups and monitoring of their condition.
Gastroparesis Risk Factors
Factors that increase the tendency to develop gastroparesis include
- Diabetes: both type 1 and 2
- Gastric surgeries: especially of the esophagus or upper abdomen
- Viral infections
- Nervous system disorder, such as Parkinson’s
- History of gastric disorders
- Cancers, too, especially when close to the abdominal region, etc.
Overall, gastroparesis is an uncommon disorder, even in diabetic patients. However, it is a diabetic complication. A report states that it is even more common in type 1 diabetes patients than in type 2.
Another report suggests that it is more likely to occur in adult females than males.
Causes: How Does Diabetes Cause Gastroparesis?
If you have been paying attention as you read through this article, we have mentioned the primary cause: vagus nerve damage.
However, people with diabetes, especially for an extended period, tend to experience an impairment of this nerve, and perhaps some other ones in the body, resulting in the condition.
Diabetes, sometimes, may impair blood vessels that are supposed to transport oxygen and nutrients. So when the blood vessels that ought to supply the vagus nerve, for example too, are affected, it may also result in this condition.
Complications
If not quickly addressed, gastroparesis may become a severe disorder. Below are some of the complications of this disorder.
Malnutrition
Lack of appetite and early satisfaction are some of the hallmarks of gastroparesis. Poor appetite may prevent you from taking adequate nutrients to sustain your body.
Irregular Changes in Blood Sugar Levels
Irregularities in food movement from the stomach into the small intestine may cause erratic spikes in blood glucose levels. Though, gastroparesis does not cause diabetes. It, however, makes treatment and management of diabetes extremely difficult.
Bezoars
Extended periods of undigested food remaining in the stomach can cause them to harden, forming solid masses known as bezoar. Bezoars may cause simple disorders like nausea and vomiting, but it may be fatal if it remains for long. It prevents food from getting into the small intestine for proper absorption.
Inflammation of the Esophagus
Gastroparesis may cause the esophagus to get inflamed, causing problems with swallowing. Also, in cases of too much vomiting, it may lead to esophagus tears. Gastroparesis needs to be taken seriously, as it may be detrimental to overall health.
Extreme Dehydration
Frequent vomiting may lead to severe dehydration and extreme thirst.
In all, gastroparesis affects the quality of life. It causes erratic spikes in blood sugar levels – it may be too high or too low. When present in people with diabetes, it makes therapy difficult. In type 1 diabetes, for example, gastroparesis, patients would find it challenging to know the appropriate time to take insulin shots.
When sugar levels are too high over extended periods, there’s an increased risk of the following in diabetic patients.
- Heart-related problems
- Digestive and kidney diseases
- Ketoacidosis
- Eye problems, especially retinopathy
- Amputation
- Neuropathy
When sugar levels are too low over, it increases the risks of the following:
- Diabetic coma – excessively low blood sugar.
- Seizures – misfiring of electrical impulses in the brain.
- Falls and shakiness.
Diagnosis
Gastroparesis often proves challenging to diagnose because of its similarities with other gastro-intestinal conditions like heartburn and acid reflux. So, if care is not taken, one may continue to treat the symptoms without necessarily addressing the primary cause.
Before diagnosing diabetic gastroparesis, your healthcare provider must have considered many factors – the signs and symptoms you complain about and your medical history, too, may prove vital in diagnosis. Your doctor may then request urine or blood tests to check for complications.
Some of the tests to confirm gastroparesis include
- Imaging tests: to check for obstructions in the abdomen and stomach.
- Barium beefsteak meal or barium x ray: it detects abnormalities in the digestive tract. It involves monitoring how long it takes for digestion to occur.
- Esophagogastroduodenoscopy (EGD): a procedure that allows the examination of the alimentary canal – esophagus, stomach, and duodenum.
- Gastric emptying scintigraphy or radioisotope gastric emptying scan: assesses the ability of the stomach to empty its contents.
Treatment and Therapy of Diabetic Gastroparesis
Control and regulation of blood sugar levels are of the utmost importance for patients with diabetic gastroparesis. Once diagnosed with diabetic gastroparesis, doctors often stress the need to monitor blood sugar levels in such patients, even more than in typical diabetes.
Therapy and treatment of the condition include:
Use of Medications
Your doctor may prescribe the following oral medications to treat gastroparesis.
- Stomach muscle stimulators.
- Antiemetics and drugs to reduce nausea vomiting.
- Use of NSAIDs for pain management.
Adjustments to the dosage and timing of insulin shots, too, may be recommended. Also, people with diabetic gastroparesis must avoid opiates and other drugs that may delay stomach emptying.
Dietary Modifications
Doctors often recommend changes in dietary plans and eating habits for people with diabetic gastroparesis. You need to avoid high fiber and fatty foods, as these foods take time to digest. Instead, focus more on liquid meals, proteins like eggs and fish; they are easily digestible. Non-starchy fruits and vegetables are also good choices.
It is also essential to chew foods well before swallowing. You may need to see a dietitian assist you in working out a suitable dietary plan for the best outcomes.
Gastric Electrical Stimulation
This is used in severe cases where a device is surgically implanted into the stomach. This device releases electrical impulses that promote the simulations of the nerves and stomach muscles.
In rare cases of gastroparesis, doctors may recommend intravenous nutrition. Here nutrients and fluids enter the blood directly, through feeding tubes bypassing the stomach. It is perfect for regulating blood sugar levels. However, this is only done in severe cases of gastroparesis.
Conclusion
Healthy nutrition is key to avoiding many metabolic disorders, including diabetic gastroparesis. Avoid junk. Instead, focus more on eating a healthy and nutritious meal.
When suffering from diabetic gastroparesis, it is, in fact, more important to monitor blood glucose levels than in one with just diabetes. You may not be able to visit your doctor often, so you need to use diabetes management apps. These apps help you keep track of your blood glucose levels. A typical example of such an app is Klinio.